For years I
was a physician to members of his family and had known this 59-year-old
executive. I was surprised when he
was admitted to our hospital for palpitations and weakness.
I knew that he
used to drink alcohol socially, and when that became a problem, he had quit
sixteen years ago. I was aware
that he took pride in his health.
He was proud that he ate organic and natural foods. At admission we learned that he
consumed nearly a quart of yogurt each day, and also each day drank ten to
twenty cups of herbal teas.
His personal physician had seen him regularly for routine
health matters. He prescribed a medication
for anxiety. He had found that his
blood pressure was high, and it proved to be somewhat difficult to treat. Three
drugs were used in a step-wide fashion during the next 18 months.
Now, because of the
palpitations and weakness, he had gone to the emergency room of our hospital
where his serum potassium was found to be 2.2 millimoles per liter. Such low levels of potassium
(hypokalemia) are dangerous and can lead to ventricular fibrillation and death. He was admitted to the hospital for
close observation and treatment.
Potassium was administered intravenously and his serum
potassium level increased somewhat to 2.8 millmoles. His
palpitations disappeared.
His hypokalemia most certainly
was the cause of his symptoms, but what was causing his potassium to be so low?
As a thiazide had recently been added to his blood pressure
medications, the hospital’s clinicians briefly considered that this might be
the culprit. However, he was on an
appropriately low dose of the thiazide that ordinarily would not cause this
level of hypokalemia.
Over the next few days he remained markedly hypokalemic despite
additional potassium. Multiple physicians examined him
for other conditions that might cause hypokalemia, particularly those which
cause hypertension too.
Hyperaldosteronism was one such diagnostic
hypothesis. Although not common,
this can be a serious disease. Hyperaldosteronism
is the over production of a salt retaining hormone, aldosterone, which may
occur from an adrenal gland tumor or from severe narrowing of an artery to the
kidney, i.e., renovascular disease.
Other less common causes of hypokalemia and hypertension were also considered,
some of them seemingly benign, such as excessive amounts of licorice in the
diet, but the patient denied a fondness for licorice.
After extensive testing,
neither hyperaldosteronism nor any other cause was found. He was a diagnostic puzzle, but, he
felt well, and he was sent home when his potassium returned to normal.
Shortly
after discharge, at the request of his in-patient internist, he brought in his
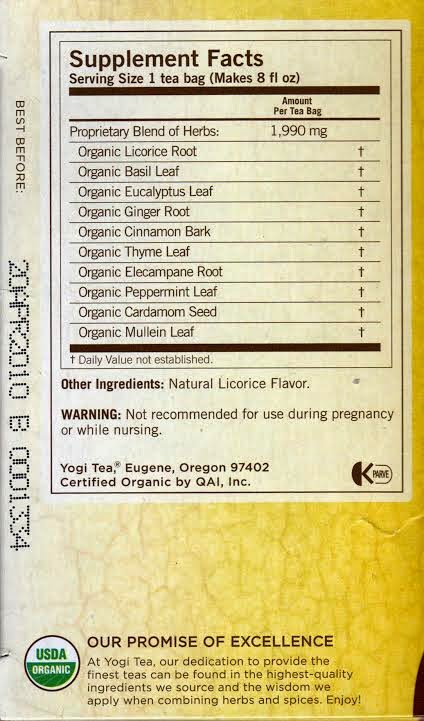
herbal teas. In each licorice root
was a major ingredient! The
mystery was solved.
As you
recall, he had mentioned at the time of his admission to the hospital that he
had been drinking ten to twenty cups of these teas per day for many
months. These were taken to
calm his nerves after tense days at the office. Even though they were intrigued
by the extraordinary amount of herbal teas that he drank each day, his
clinicians were unaware that some herbal teas contain licorice. He had denied licorice use.
He stopped
drinking the teas. He was seen
again in the clinic thirty days after discharge and he said he felt
terrific. His blood pressure was
104/64 and his serum potassium was 5.1 millimoles per liter. Antihypertensive medications were
reduced and eventually discontinued.
Eating
licorice is an uncommon cause of the syndrome of hypertension and hypokalemia. In
the past few decades with the virtual disappearance in the United State of
candy that contains true licorice root; it has virtually disappeared. However, it is important to note
that other sources of true licorice root are still available. These sources, including herbal teas,
should be considered in patients with unexplained hypertension and
hypokalemia.